Action Under the Law of Torts
The Law of Torts provides a legal remedy for compensating victims who have suffered injury or loss due to the wrongful acts of others, including medical malpractice. Medical negligence, being a civil wrong, is actionable in civil courts under tort law. However, proving negligence in medical cases is a high burden for the plaintiff, as the court requires strict evidence.
To successfully claim compensation under the law of torts, the following key elements must be demonstrated:
- Duty of Care: The medical professional owed a duty of care to the patient.
- Breach of Duty: The medical professional failed to meet the required standard of care.
- Damages: The breach resulted in actual harm or damage to the patient.
However, simply proving these elements is not enough. The plaintiff must provide cogent evidence that establishes negligence. This often involves expert testimony from medical professionals and the submission of medical records to corroborate the patient’s claims. Without clear evidence of negligence, the case will likely fail.
Action Under the Law of Contracts
Under the Law of Contracts, the scope for holding a healthcare professional liable for medical negligence is more limited compared to tort law. When a patient seeks medical care from a healthcare provider, a contractual relationship is formed. This is usually an implied contract, where the doctor agrees to provide treatment in exchange for payment (either directly or through insurance, etc.).
However, in the context of medical malpractice, a lawsuit under the law of contracts can only be filed if:
- Consideration: The patient has availed of the healthcare provider’s services for a consideration (payment or insurance claim).
- Existence of a Contractual Obligation: There is an explicit or implied contractual obligation between the patient and the healthcare provider.
A civil suit for breach of contract will not be maintainable unless the plaintiff proves that a contractual relationship existed. This means that if a patient did not directly hire the doctor or sign a contract, it may be difficult to bring a claim for negligence under contract law. The relationship between the patient and doctor, therefore, must be proven to be contractual, based on the services provided and payment made.
In summary, compensatory actions for medical negligence can be pursued either under the law of torts or contracts, but each route requires a different approach and evidentiary standards. The law of torts generally offers broader scope for compensation, while the law of contracts is more restrictive, requiring clear proof of a contractual obligation and consideration.
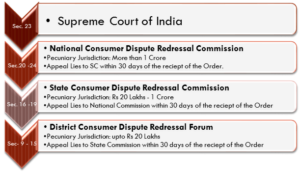
HEIRARCHY FOR CONSUMER DISPUTES REDERESSAL COMMISSIONS UNDER CONSUMER PROTECTION ACT, 1986
Remedy Under the Consumer Protection Act, 1986
Introduction
The Consumer Protection Act, 1986 (CPA) provides a legal framework for the protection of consumer rights in India, ensuring that consumers who suffer harm due to deficiency of services can seek redress. If a medical practitioner, hospital, or healthcare provider is found to have rendered deficient service that resulted in harm to a patient, the patient can file a complaint under the CPA. The Act provides three levels of quasi-judicial bodies for dispute resolution: the District Forum, State Commission, and National Commission.
Deficiency of Service
Under the Consumer Protection Act, deficiency of service is defined as any fault, imperfection, shortcoming, or inadequacy in the quality, nature, or manner of performance of a service. This includes services rendered by medical professionals, hospitals, or nursing homes. A deficiency can occur due to improper treatment, negligence, or failure to meet the standards expected of a medical provider. The Act mandates that services must be performed in accordance with any relevant laws and the terms agreed upon in a contract, either implied or explicit.
Patient as a Consumer
To file a complaint against a medical practitioner under the Consumer Protection Act, the patient must meet the definition of a consumer as stipulated in the Act. The definition of a consumer under the CPA includes individuals who have:
- Hired or availed of services for a consideration.
- Had the service rendered to them.
- Paid or promised to pay consideration for the service.
Therefore, a patient must have hired the medical service and paid for it, either directly or indirectly, for them to be considered a consumer. Importantly, if medical services are provided free of charge, as in the case of treatment in government hospitals or charitable institutions, the patient is not considered a consumer under the Act. This exception is crucial when considering medical negligence claims.
Medical Services Covered Under the Act
The services rendered by medical professionals, hospitals, or nursing homes must fall within the definition of “service” under Section 2(1)(i) of the Consumer Protection Act to be actionable. This section defines “service” as any description of service made available to potential users, excluding free services or services under personal service contracts.
In the case of IMA v. V.P. Shantha and others, the Supreme Court of India clarified that medical services provided by doctors, hospitals, and nursing homes are covered under Section 2(1)(i) of the Consumer Protection Act. However, this excludes free medical services or services provided under personal service contracts.
This means that a patient who has paid for treatment or availed of medical services for a fee is a consumer and can seek remedy under the Act if they suffer from deficient medical care. However, services rendered free of charge or under a personal contract (e.g., a family doctor offering unpaid services) do not fall under the purview of the Consumer Protection Act.
Remedy Under the Constitution of India
While the Constitution of India does not explicitly grant special rights to patients, the right to health and medical treatment can be inferred from the broad scope of Article 21 of the Constitution, which guarantees the right to life and personal liberty. The right to life would be meaningless unless medical care is assured to a sick person. Hence, a breach of this right due to negligent medical care can render healthcare providers liable for their actions.
Article 19(1) guarantees certain fundamental freedoms to all citizens, including the freedom to live with dignity. The exercise of these freedoms is inherently tied to the health and well-being of individuals. A person cannot fully enjoy these freedoms without proper medical care, which is implicitly protected under Article 21.
Therefore, if a person’s health is compromised due to medical negligence, it can be seen as a violation of their right to life under Article 21. In such cases, the healthcare provider may be held liable for failing to uphold this fundamental right, and the victim can seek legal remedy for the breach.
The Consumer Protection Act, 1986 provides a vital legal framework for patients who suffer from medical negligence to seek redress and compensation. By defining medical services as a form of service under the Act, it allows patients who have paid for healthcare services to pursue claims in consumer forums. Additionally, the Constitution of India offers a broader interpretation of the right to health under Article 21, making healthcare providers liable for negligence that violates a patient’s right to life. Together, these legal provisions ensure that patients can access remedies when their rights are violated due to medical malpractice or negligence.
Criminal Negligence under Section 304-A of the Indian Penal Code (IPC)
Introduction to Criminal Negligence
Section 304-A of the Indian Penal Code (IPC) deals with causing death by a rash or negligent act not amounting to culpable homicide. To hold someone criminally liable under this section, it is necessary to establish that the death was a direct result of the accused’s rash or negligent actions. The death must be the proximate cause, meaning the immediate or operating cause, without intervention from other factors. This section does not apply to cases where the accused’s actions were simply a necessary or inevitable cause (causa sine qua non).
Criminal liability under Section 304-A arises from acts that show a reckless disregard for human life or gross negligence. There is a critical distinction between rashness and negligence:
- Rashness: An act done with the awareness of risk and knowledge that harmful consequences might follow but proceeding with the act regardless, often due to recklessness or indifference.
- Negligence: The failure to exercise reasonable care to avoid harm. This is often an omission to take precautions that a reasonable person would have taken.
The key to criminal liability under Section 304-A is that the negligence or rashness must be of such a degree that it could be described as gross negligence or recklessness, leading to a criminal act.
Rash or Negligent Act in Medical Treatment
In the context of medical treatment, a doctor can be prosecuted under Section 304-A if a rash or negligent act causes the death of a patient. This could occur, for example, when a doctor performs an operation that they are not qualified to conduct or fails to take necessary precautions during a procedure.
The Supreme Court of India has set a high standard of negligence for criminal liability in medical negligence cases. The level of negligence required is not simply a lack of care; it must be gross negligence or recklessness, beyond a mere error in judgment or an accident. In other words, for a doctor to face criminal liability under this section, their conduct must be so egregiously negligent that it demonstrates disregard for life and safety, which goes beyond simple incompetence or error.
Degree of Negligence
To hold a medical professional criminally liable for negligence, it must be proven that their actions or inactions were so egregious that no reasonable medical practitioner would have done or failed to do the same under the same circumstances. It must be shown that the act was done with a reckless disregard for the safety of the patient, and that it was highly likely to cause harm.
The Supreme Court in the Dr. Suresh Gupta Case (2004) clarified that while a doctor may be civilly liable for compensation in cases of medical negligence, criminal liability under Section 304-A arises only when the negligence is gross and the act is so reckless that it endangers the life of the patient. It is not sufficient for the death to be a result of an error in judgment; it must be a direct consequence of criminal negligence or recklessness.
Disciplinary Action
In addition to criminal liability, medical professionals can face disciplinary action by the relevant medical councils. The Medical Council of India (MCI) regulates the professional conduct of doctors and other healthcare providers in India. The MCI and state medical councils have the authority to take action against doctors found guilty of serious professional misconduct.
Grounds for Disciplinary Action
Disciplinary action can be initiated if the medical practitioner is found guilty of:
- Conviction of a criminal offense by a court of law, particularly one involving moral turpitude.
- Professional misconduct that tarnishes the reputation and integrity of the medical profession, such as:
- Adultery or improper conduct with a patient.
- Issuing false certificates, reports, or documents.
- Issuing a certificate of efficiency in modern medicine to an unqualified person.
- Performing an illegal abortion or surgery without medical necessity.
- Disclosing a patient’s identity without consent.
- Performing an operation that leads to sterility without obtaining prior written consent from the patient.
- Refusing medical assistance solely on religious grounds.
Such actions are considered serious professional misconduct, and if a doctor is found guilty of these offenses, the medical council may take corrective steps, which may include removal from the medical register for a specified period or even permanently in severe cases.
Section 304-A of the IPC provides a legal framework for prosecuting individuals who cause death by rash or negligent acts. In medical practice, a doctor can face criminal charges under this section if their negligence or recklessness results in the death of a patient. However, the standard for criminal negligence is high, and the act must be deemed grossly negligent or reckless. Furthermore, medical professionals are subject to disciplinary actions by medical councils if their conduct violates professional ethics or legal standards. Such actions may range from warnings to removal from the medical register, depending on the severity of the misconduct.
Recommendatory Action: Complaints Before Human Rights Commissions
In addition to the various legal remedies available to patients who suffer from medical negligence, there exists an alternative mechanism to protect patient rights through the National Human Rights Commission (NHRC) and State Human Rights Commissions (SHRC). These commissions are established to safeguard the human rights of individuals, ensuring that their basic rights, including the Right to Life, are respected and protected.
Role of Human Rights Commissions in Medical Negligence
Irrespective of an individual’s caste, creed, religion, or economic status, every patient is entitled to the protection of their human rights. The NHRC and SHRC serve as guardians of these rights, especially when they are violated by state agencies, including public hospitals or government healthcare providers. In cases of medical negligence, a patient or their family may file complaints with the NHRC or SHRC if they believe that their right to health or right to life has been violated.
How NHRC/SHRC Can Help
- Filing Complaints: Patients can approach the NHRC or SHRC to report violations of their human rights. These complaints may involve issues such as negligence in healthcare delivery, lack of proper treatment, or failure by the state to ensure adequate medical facilities.
- Investigation and Accountability: Once a complaint is lodged, the NHRC or SHRC has the authority to conduct independent investigations into the matter. They can issue summons to witnesses, examine evidence on oath, and take necessary steps to determine if the violation occurred.
- Power of Civil Court: NHRC and SHRC have powers akin to a Civil Court, allowing them to enforce their findings. They can request explanations from the government or health authorities responsible for the violation and seek redress for the affected parties.
- Compensation and Interim Relief: In cases of confirmed human rights violations, NHRC and SHRC may recommend that the government or healthcare institution provide compensation to the victim or their family. They can also recommend the payment of interim relief while the investigation is ongoing to provide immediate support to the affected patient or their family members.
Importance of Human Rights Commissions
- Oversight Role: NHRC and SHRC play a significant role in holding the state accountable for violations of human rights in healthcare. By ensuring that the government adheres to national and international human rights standards, they help in the fulfillment of patients’ rights to health.
- Promoting Awareness: The work of the Human Rights Commissions also serves to raise public awareness about the rights of patients and the need for accountability in medical practice. This can lead to a more patient-centered approach in the healthcare system.
- Protection from Institutional Negligence: The commissions offer a crucial platform for individuals who may feel powerless against large healthcare institutions or the government, ensuring that they can seek justice even when other legal avenues may seem inaccessible or ineffective.
Human Rights Commissions, both at the national and state level, provide an essential mechanism for protecting patients’ rights in cases of medical negligence. They not only hold the state accountable for violations but also ensure that victims receive compensation and interim relief. By empowering patients to file complaints and seek justice, NHRC and SHRC contribute to the broader effort of ensuring healthcare as a fundamental human right.